Sitting Is The New Smoking
With a large number of individuals remotely working from home due to Covid-19 restrictions, a consequence of this is having difficulty separating work life from personal life, especially when both take place in the same area. We unintentionally may spend more hours sitting at a desk which over time can lead to an array of adverse health risks such as increased risk of cardiovascular disease, obesity, cancer, metabolic diseases such as diabetes mellitus, hypertension, musculoskeletal diseases such as osteoporosis and poor posture (Park et al, 2020). This article chronicles poor posture being detrimental to our health, and lifestyle modifications we can make to facilitate the longevity of our spine and enhance our health and wellbeing.
The way we sit, stand and walk has a long term effect on our musculo-skeletal system (Swann, 2009). A person with good posture will be able to keep their spine in proper alignment whilst carrying out their everyday activities. They will have adequate sensory feedback which means the brain will be aware of where their limbs are in space along with a good sense of equilibrium to maintain good balanced posture. (Swann, 2009). Prolonged poor sitting overtime can lead to poor posture which can lead to muscular and joint pain especially in the neck, shoulders and lower back (Swann, 2009). This is because the joints will be working in an abnormal pattern, causing the ligaments to stretch reducing the efficiency of the joint. When the surfaces of the joints are not aligned correctly this results in abnormal load-bearing on the joints and ligaments.
This can hasten the degenerative changes on the joints surface resulting in osteoarthritis (Swann, 2009). Poor posture is also known to impact the skeletal muscle.
Skeletal muscle can be categorized as fast twitch or slow twitch. (Department of Health, 2015). The slow twitch muscle fibers are found in the deeper muscle layers where they contain sensory receptors that relay information to the brain about body awareness and hence are responsible for posture and balance. This muscle fiber is designed to keep working for long durations without tiring. (Department of Health, 2015). Whereas, the fast twitch muscle fibers are responsible for movement and activity and tire out quickly. (Department of Health, 2015).
With poor posture, the fast twitch muscle fibers are activated resulting in muscle fatigue as they are not designed to be activated for prolonged periods. In contrast, the slow twitch muscle fibers waste away from the lack of use. The atrophied muscles tighten up and shorten putting extra pressure on the spine to hold the body upright resulting in worsened posture. (Department of Health, 2015).
As mentioned earlier, the slow twitch muscle fibers are responsible for proprioception and relaying this information back to the brain. With the slow twitch muscle fibers wasting away and the fast twitch muscle fibers acting as the dominating muscle fiber in maintaining posture, the brain gets an incomplete picture about body awareness and thus counteracts this by contracting the muscles further which can add to general fatigue and pain. (Department of Health, 2015).
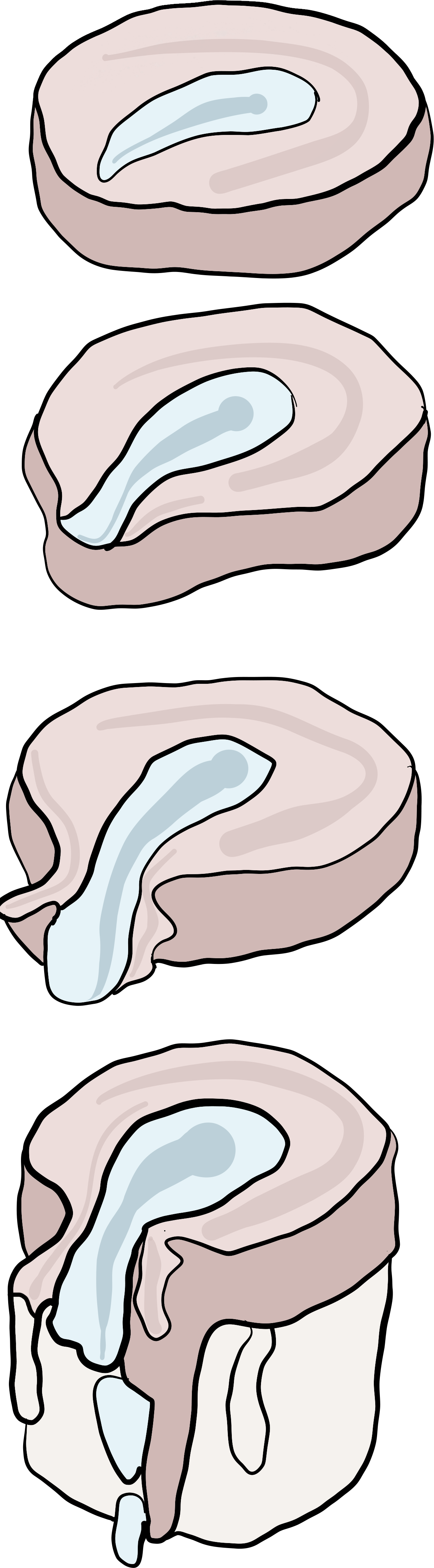
When sitting at a desk for a prolonged period of time, this begins to train your nervous system to hold incorrect postural alignment. The muscles in the front of your neck become chronically shortened, while the muscles in the back of your neck lengthen. This constant biomechanical position causes the joints in the spine of the neck to change which usually results in a forward head posture, also known as the text neck (Neupane et al, 2017).
Sedentary behavior can also change the balance of your pelvis. The hamstrings, gluteal muscles and abdominal muscles can weaken and lengthen whereas the back extensors and hip flexors shorten and tighten causing the pelvis to tilt forward. When the gluteal muscles lengthen, they have delayed activation and thus the smaller muscles now try to take over the job of the gluteal muscles, which don’t have the size or metabolism to do so and thus fatigue quickly. (Puagprakong et al, 2021).
Lifestyle Modifications:
Ergonomically correct workstation (Corlett, 2009).
● Sit as close as possible to your desk
● Elbows should be at a 90 degree angle. If elbows are not at 90 degrees you need to move the chair up or down
● Thighs should be parallel to the floor, if your thighs are parallel to the floor you should be able to slide your fingers under your thigh at the edge of the chair. If your fingers cannot glide through a footrest will be required to elevate the feet. If your fingers slide easily then the chair needs to be raised
● Calves- With your buttocks right against the back of the chair a clenched fist should be able to pass through the back of the calf and the front of the chair. If not, this indicates that the chair is too deep and the backrest will need to come forward
● Lower back support- A lumbar support pillow should be used to prevent slouching in your chair when you tire as this can put extra stress on your spine
● Eye level- Gaze should be aimed at the center of the computer screen to prevent tilting of the neck/head, it is also recommended to get up and move every 30 minutes to prevent shifting into a poor sitting posture but also to reactivate the muscles and reduce discomfort. (Davis et al, 2014)
How Chiropractic Care Can Help
Postural changes are known to affect the structural integrity of the spine. This means that the bones that make up the spine aren’t moving as they should. This affects the surrounding spinal muscles which contain sensory receptors that act as “eyes for the brain.”
Areas of spinal dysfunction will cause the surrounding muscles to act as protective muscles instead and will send incorrect signals to the brain about the body. The brain will perceive these signals as normal and adapt to it causing an inflammation process in that area. Chiropractors will find those dysfunctional areas and perform a high velocity, low amplitude adjustment. This will stretch the surrounding muscles and help re-establish normal processing within the brain. This will allow the brain to have greater awareness of what’s going on in the body, help in the prevention of muscle fatigue and help in the proper alignment of the spine. (Haavik et al, 2021).
What To Expect At Your First Chiropractic Visit
An initial Chiropractic exam for back pain will typically have three parts: a consultation, case history, and physical examination. Laboratory analysis and X-ray examination may be performed.
Consultation. The patient meets with the chiropractor and provides a brief synopsis of his or her lower back pain, such as:
Duration and frequency of symptoms
Description of the symptoms (e.g. burning, throbbing)
Areas of pain
What makes the pain feel better (e.g. sitting, stretching)
What makes the pain feel worse (e.g. standing, lifting).
Case history. The chiropractor identifies the area(s) of complaint and the nature of the back pain by asking questions and learning more about different areas of the patient's history, including:
Family history
Dietary habits
Past history of other treatments (chiropractic, osteopathic, medical and other)
Occupational history
Psychosocial history
Other areas to probe, often based on responses to above questions
Physical examination. A chiropractor may utilize a variety of methods to determine the spinal segments that require chiropractic treatments, including but not limited to static and motion palpation techniques determining spinal segments that are hypo mobile (restricted in their movement) or fixated. Depending on the results of the above examination, a chiropractor may use additional diagnostic tests, such as:
X-ray to locate subluxations (the altered position of the vertebra)
A device that detects the temperature of the skin in the paraspinal region to identify spinal areas with a significant temperature variance that requires manipulation.
Chiropractors are trained in a variety of methods to assess the underlying cause of the problem, including:
Evaluation and management services. Chiropractors are trained in examining the joints, bones, muscles and tendons of the spine, head, extremities and other areas of the body with the purpose of noting any misalignment, tenderness, asymmetry, defects or other problems.
Neurologic and other common physical examination procedures. Chiropractors are trained to perform a variety of neurologic tests (nerve root compression/tension, motor strength, coordination, deep tendon and pathological reflexes, etc.) and are skilled in performing orthopedic, cardiovascular and many other common examinations.
Specialised assessment. Chiropractors are trained to assess range of motion, stability, muscle strength, muscle tone and other assessments with the lower back.
Common diagnostic studies. Chiropractors are trained in use of diagnostic studies and tools such as radiography (X-rays), laboratory diagnostics and neurodiagnostics.
References
1. Park, J. H., Moon, J. H., Kim, H. J., Kong, M. H., & Oh, Y. H. (2020). Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean journal of family medicine, 41(6), 365–373. https://doi.org/10.4082/kjfm.20.0165
2. Bond, M. (2006). The new rules of posture: How to sit, stand, and move in the modern world. Simon and Schuster. Department of Health, State Government of Victoria, Australia. (2015). Better Health Channel, Posture.Retrieved on 22 Jan from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/posture#two-types-of-muscle-fibres
3. Corlett, E. N. (2009). Ergonomics and sitting at work. Work, 34(2), 235-238 https://pubmed.ncbi.nlm.nih.gov/20037235/
4. Swann, J. (2009). Good positioning: the importance of posture. Nursing And Residential Care, 11(9), 467-469 http://www.julieswann.com/NRC1109.pdf
5. Neupane, S., Ali, U. I., & Mathew, A. (2017). Text neck syndrome-systematic review. Imperial Journal of Interdisciplinary Research, 3(7), 141-148 https://www.semanticscholar.org/paper/Text-Neck-Syndrome-Systematic-Review-Neupane-Ali/d4d58fd3e1b10bb6276b926917dc5d2c6d633cab
6. Puagprakong, P., Earde, P., & Kooncumchoo, P. (2021, April). Lumbo-Pelvic-Hip Angle Changes During Upright and Free Style Sitting in Office Workers with Lower Crossed Syndrome. In International Conference on Human Interaction and Emerging Technologies (pp. 532-538). Springer, Cham https://www.researchgate.net/publication/350916643_Lumbo-Pelvic-Hip_Angle_Changes_During_Upright_and_Free_Style_Sitting_in_Office_Workers_with_Lower_Crossed_Syndrome
7. Davis, K. G., & Kotowski, S. E. (2014). Postural variability: an effective way to reduce musculoskeletal discomfort in office work. Human factors, 56(7), 1249-1261 https://pubmed.ncbi.nlm.nih.gov/25490805/
8. Haavik, H., Kumari, N., Holt, K., Niazi, I. K., Amjad, I., Pujari, A. N., ... & Murphy, B. (2021). The contemporary model of vertebral column joint dysfunction and impact of high-velocity, low-amplitude controlled vertebral thrusts on neuromuscular function. European Journal of Applied Physiology, 1-46 https://pubmed.ncbi.nlm.nih.gov/34164712/