5 Top Causes Of Back Pain
Day to day stress such as sitting for long periods, driving and poor posture can lead to ongoing stress throughout your body. The stress is usually silent until it builds up and causes an overload to your body which sometimes can be irreversible. There are many causes of back pain, here are the top causes:
#1
Sprain/Strain
A sprain means an injury to a ligament, and ligaments support the spine, including its joints—the facet joints. A strain is a muscle and/or tendon injury. Tendons connect muscle to a bone. A spinal sprain or strain can happen if you fall, use poor body mechanics (eg, lifting and twisting simultaneously), during a car accident, and many other ways. These are usually quite painful and may temporarily limit movement.
#2 Spinal Nerve Compression
When a spinal nerve root is compressed, entrapped, or pinched it becomes inflamed and starts to send messages the brain interprets as pain. In the illustration (below) of a cervical (neck) spine segment, many different disorders are causing nerve compression: a herniated disc, thickened ligament, and bone spurs (also called osteophytes).
#3
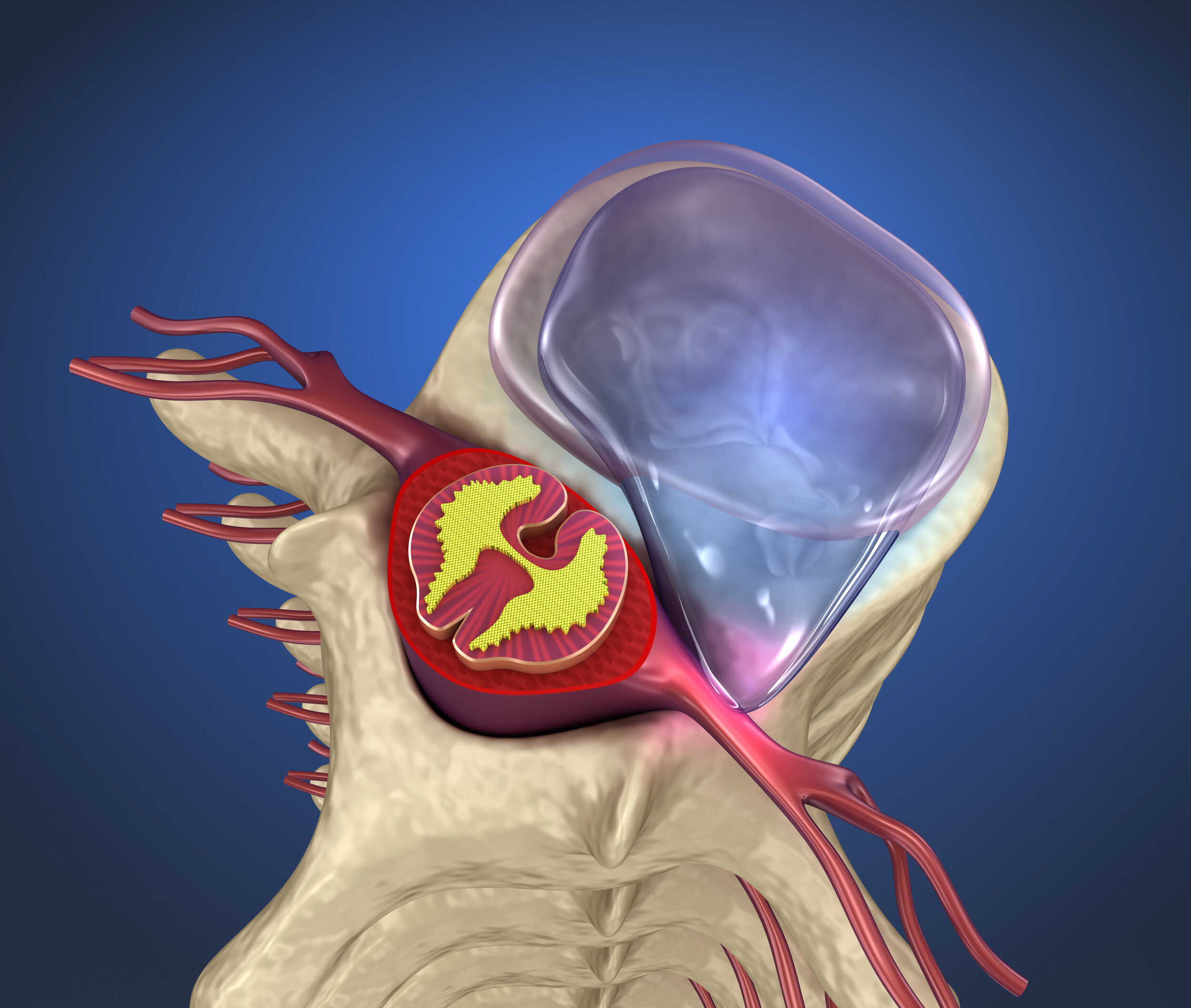
Lumbar Herniated or Bulging Disc
A herniated disc is illustrated in the picture above. There the contents of the disc (nucleus pulposus) have spilled out through the disc’s tough protective outer layer (annulus fibrosus). The nucleus pulposus is compressing a spinal nerve root and may cause back pain, with or without leg pain. Depending on the severity of nerve compression or damage, and where in the lower back the disc herniation has occurred, the patient may develop buttock, thigh, and leg pain. The location of back pain is generally diffuse and not located in a specific area. However, leg pain typically follows specific dermatomal patterns consistent with specific nerve root irritation.
The patient may be told they have sciatica. The term sciatica is used to describe a group of symptoms that develop when the sciatic nerve is compressed.
True sciatica is represented by pain following a specific nerve root pattern.
Typical lower back, buttock and proximal (nearby) thigh pain are commonly called sciatica but the sciatic nerve gives off no major branches above the knee.
#4
Degenerative Disc Disease
This typifies many age-related spine problems. It is not really a disease but rather helps to describe the changes spinal components undergo as a result of growing older. As we grow older, our bodies undergo changes at the cellular levels. A facial wrinkle is an example of a degenerative cellular change.
As we age, the intervertebral discs begin to dehydrate (water volume diminishes); their shape and height may change affecting the space between two vertebral bodies (disc space). When disc space is reduced, a nerve passageway (neuroforamen) narrows.
The disc and facet joints work in tandem. Abnormal stresses applied to the disc are transferred to the facets resulting in overgrowth of capsular ligaments, formation of osteophytes, and reduction in facet joint movement. While all this is going on, the body is trying to find a way to stop abnormal movement, heal itself. Cartilage on the facet joints may wear away. Basically, a slow degenerative cascade develops. Bone spurs develop and may further impinge nerve roots within the foramen and or spinal canal.
#5
Sacroiliac Joint Dysfunction
The “keystone” of the pelvis is the sacrum. Where the sacrum and the ilium meet at the left and right sides of the back are the sacroiliac (SI) joints. These joints are supported by strong ligaments. The actual amount of joint movement is very small. SI joints may move too much or not enough. When the SI joint does not function properly, the symptoms include lower back pain and proximal leg pain.
Examples of Uncommon Causes of Back Pain
Spinal infections are a less common cause of back pain. These infections can be bacterial or fungal and can affect the intervertebral discs, spinal bone (osteomyelitis), spinal cord, or area around the nerve roots (epidural space).
Spinal Tumors are benign (not cancer) or malignant (cancer). These abnormal growths (called neoplasms) can be primary or metastatic. A primary spinal tumor is one that originates in the spine—within a vertebral body, nerve roots, or spinal cord. Metastatic tumors are those that have migrated from another part of the body—such as a breast, kidney, or lung.
Chiropractic Care
Chiropractic adjustments can help to relieve pressure within the body by realigning areas that have moved out of place due to stress. Chiropractic care can help to prevent future issues from occurring and in turn can help to keep your spine healthy, therefore allowing you to do and be more.
References
https://www.spineuniverse.com/conditions/back-pain/common-uncommon-causes-back-pain
Danielle A.van der WindtPhD(Professor of Primary Care Epidemiology)
Kate M.DunnPhD(Reader in Epidemiology)1 https://www.sciencedirect.com/science/article/abs/pii/S1521694213000971
https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/low-back-pain-fact-sheet
Low back pain in patients with multiple sclerosis: A systematic review and the prevalence in a French multiple sclerosis population
C.MassotaC.DonzeaM.-A.GuyotaS.Leteneurbcd https://www.sciencedirect.com/science/article/pii/S0035378720306834
Clinical and radiographic features of spinal osteoarthritis predict long-term persistence and severity of back pain in older adults
Roxannevan den BergaAlessandroChiarottoaWendy T.EnthovenaEveliende SchepperaEdwin H.G.OeibBart W.KoesaSita M.A.Bierma-Zeinstraac https://www.sciencedirect.com/science/article/abs/pii/S1877065720301536
Back pain in children lPrasadKarpeMaire-ClaireKillenDavidFender https://www.sciencedirect.com/science/article/abs/pii/S0263931920301460
Back pain in surgically treated degenerative lumbar spondylolisthesis: what can we tell our patients?
MichaelBondMD, FRCSCaNathanEvaniewMD, FRCSCagChristopher SBaileyMD, FRCSCbRaymond AndrewGlennieMD, FRCSCcJeromePaquetMD, FRCSCdNicolasDeaMD, FRCSCaHamiltonHallMD, FRCSCeNeilMansonMD, FRCSCflKenThomasMD, FRCSCgGregMcIntoshMSchAlexSoroceanuMD, FRCSCgEdwardAbrahamMD, FRCSCflMichaelJohnsonMD, FRCSCiStephenKingwellMD, FRCSCjRaphaeleCharest-MorinMD, FRCSCaSeanChristieMD, FRCSCkY RajaRampersaudMD, FRCSCeCharles GFisherMD, MHSc, FRCSCaCanadian Spine Outcome and Research Network https://www.sciencedirect.com/science/article/abs/pii/S1529943020310366
Correlation between non-specific chronic low back pain and physical factors of lumbar and hip joint in office workers
DooChulShin https://www.sciencedirect.com/science/article/abs/pii/S0306987720324397
The therapeutic management of back pain with and without sciatica in the emergency department: a systematic review
JaneAshbrookaNikolaosRogdakisbMichael J.CallaghanacGillianYeowellaPeter CharlesGoodwina https://www.sciencedirect.com/science/article/abs/pii/S0031940620303916
Bialosky JE, George SZ, Horn ME, et al. Spinal manipulative therapy-specific changes in pain sensitivity in individuals with low back pain (NCT01168999). Journal of Pain. 2014;15(2):136-148.
Biller J, Sacco RL, Albuquerque FC, et al. Cervical arterial dissections and association with cervical manipulative therapy: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(10):3155-3174.
Black LI, Barnes PM, Clarke TC, Stussman BJ, Nahin RL. Use of yoga, meditation, and chiropractors among U.S. children aged 4–17 years. NCHS Data Brief, no 324. Hyattsville, MD: National Center for Health Statistics. 2018.
Boyle E, Côté P, Grier AR, et al. Examining vertebrobasilar artery stroke in two Canadian provinces. Journal of Manipulative and Physiological Therapeutics. 2009;32(2 Suppl):S194-S200.
Bronfort G, Evans R, Anderson AV, et al. Spinal manipulation, medication, or home exercise with advice for acute and subacute neck pain: a randomized trial. Annals of Internal Medicine. 2012;156(1 Pt 1):1-10.
Bronfort G, Haas M, Evans R, et al. Effectiveness of manual therapies: the UK evidence report. Chiropractic & Osteopathy. 2010;18:3.
Bronfort G, Haas M, Evans R, et al. Evidence-informed management of chronic low back pain with spinal manipulation and mobilization. Spine Journal. 2008;8(1):213-225.
Cassidy JD, Boyle E, Côté P, et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Journal of Manipulative and Physiological Therapeutics. 2009;32(2 Suppl):S201-S208.
Chaibi A, Tuchin PJ, Russell MB. Manual therapies for migraine: a systematic review. Journal of Headache and Pain. 2011;12(2):127-133.
Clarke TC, Barnes PM, Black LI, Stussman BJ, Nahin RL. Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over. National health statistics reports; no. 325. Hyattsville, MD: National Center for Health Statistics. 2018.
Furlan AD, Yazdi F, Tsertsvadze A, et al. Complementary and Alternative Therapies for Back Pain II. Evidence Report/Technology Assessment, no. 194. Rockville, MD: Agency for Healthcare Research and Quality; 2010. AHRQ publication no. 10(11)-E007.
Goertz CM, Long CR, Vining RD, et al. Effect of usual medical care plus chiropractic care vs usual medical care alone on pain and disability among US service members with low back pain: a comparative effectiveness clinical trial.(link is external)JAMA Network Open. 2018;1(1):e180105.
Gross A, Langevin P, Burnie SJ, et al. Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane Database of Systematic Reviews. 2015;(9):CD004249. Accessed at https://www.cochranelibrary.comon August 13, 2018.
Haas M, Vavrek D, Peterson D, et al. Dose-response and efficacy of spinal manipulation for care of chronic low back pain: a randomized controlled trial. Spine Journal. 2014;14(7):1106-1116.
Haynes MJ, Vincent K, Fischhoff C, et al. Assessing the risk of stroke from neck manipulation: a systematic review. International Journal of Clinical Practice. 2012;66(10):940-947.
Hebert JJ, Stomski NJ, French SD, et al. Serious adverse events and spinal manipulative therapy of the low back region: a systematic review of cases. Journal of Manipulative and Physiological Therapeutics. 2015;38(9):677-691.
Hondras MA, Linde K, Jones AP. Manual therapy for asthma. Cochrane Database of Systematic Reviews. 2005;(2):CD001002. [edited 2011]. Accessed at www.cochranelibrary.comon August 13, 2018.
Lewis RA, Williams NH, Sutton AJ, et al. Comparative clinical effectiveness of management strategies for sciatica: systematic review and network meta-analyses. Spine Journal. 2015;15(6):1461-1477.
National Institute of Arthritis and Musculoskeletal and Skin Diseases. Back Pain. National Institute of Arthritis and Musculoskeletal and Skin Diseases website. Accessed at http://www.niams.nih.gov/health_info/back_pain/default.asp on September 12, 2018.
Oliphant D. Safety of spinal manipulation in the treatment of lumbar disk herniations: a systematic review and risk assessment. Journal of Manipulative and Physiological Therapeutics. 2004;27(3):197-210.
Paanalahti K, Holm LW, Nordin M, et al. Adverse events after manual therapy among patients seeking care for neck and/or back pain: a randomized controlled trial. BMC Musculoskeletal Disorders. 2014;15:77.
Paige NM, Miake-Lye IM, Booth MS, et al. Association of spinal manipulative therapy with clinical benefit and harm for acute low back pain. Systematic review and meta-analysis. JAMA. 2017;317(14):1451-1460.
Rubinstein SM, Terwee CB, Assendelft WJ, et al. Spinal manipulative therapy for acute low-back pain. Cochrane Database of Systematic Reviews. 2012;(9):CD008880. Accessed at https://www.cochranelibrary.comon August 13, 2018.
Rubinstein SM, van Middelkoop M, Assendelft WJ, et al. Spinal manipulative therapy for chronic low-back pain. Cochrane Database of Systematic Reviews. 2011;(2):CD008112. Accessed at https://www.cochranelibrary.comon August 13, 2018.
Schneider M, Haas M, Glick R, et al. Comparison of spinal manipulation methods and usual medical care for acute and subacute low back pain: a randomized clinical trial. Spine. 2015;40(4):209-217.
Skelly AC, Chou R, Dettori JR, et al. Noninvasive nonpharmacological treatment for chronic pain: a systematic review. Comparative Effectiveness Review No. 209. AHRQ Publication No 18-EHC013-EF. Rockville, MD: Agency for Healthcare Research and Quality; June 2018.
Stussman BJ, Black LI, Barnes PM, Clarke TC, Nahin RL. Wellness-related use of common complementary health approaches among adults: United States, 2012. National health statistics reports; no 85. Hyattsville, MD: National Center for Health Statistics. 2015.
Terhorst L, Schneider MJ, Kim KH, et al. Complementary and alternative medicine in the treatment of pain in fibromyalgia: a systematic review of randomized controlled trials. Journal of Manipulative and Physiological Therapeutics. 2011;34(7):483-496.
Todd AJ, Carroll MT, Robinson A, et al. Adverse events due to chiropractic and other manual therapies for infants and children: a review of the literature. Journal of Manipulative and Physiological Therapeutics. 2015;38(9):699-712.
Vohra S, Johnston BC, Cramer K, et al. Adverse events associated with pediatric spinal manipulation: a systematic review. Pediatrics. 2007;119(1):e275-e283.
Whedon JM, Song Y, Mackenzie TA, et al. Risk of stroke after chiropractic spinal manipulation in Medicare B beneficiaries aged 66 to 99 years with neck pain. Journal of Manipulative and Physiological Therapeutics. 2015;38(2):93-101.