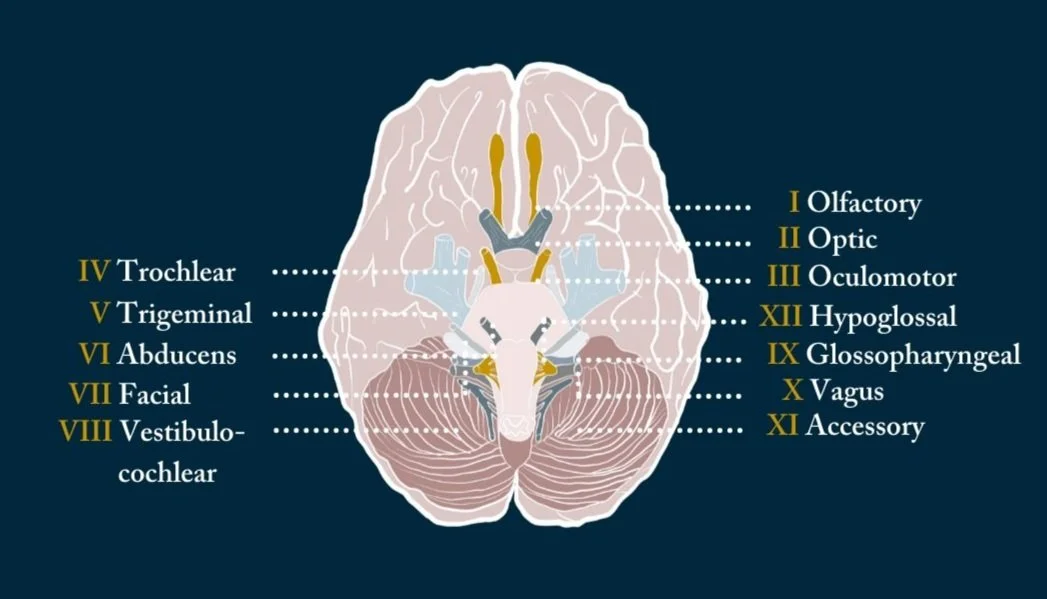
The Twelve Cranial Nerves
The cranial nerves are a set of twelve nerves that originate in the brain. Each has a different function for sense or movement.
The functions of the cranial nerves are sensory, motor, or both:
Sensory cranial nerves help a person to see, smell, and hear.
Motor cranial nerves help control muscle movements in the head and neck.
Each nerve has a name that reflects its function and a number according to its location in the brain. Scientists use Roman numerals from I–XII to label the cranial nerves in the brain.
This blog will explore the functions of the cranial nerves and provide a diagram.
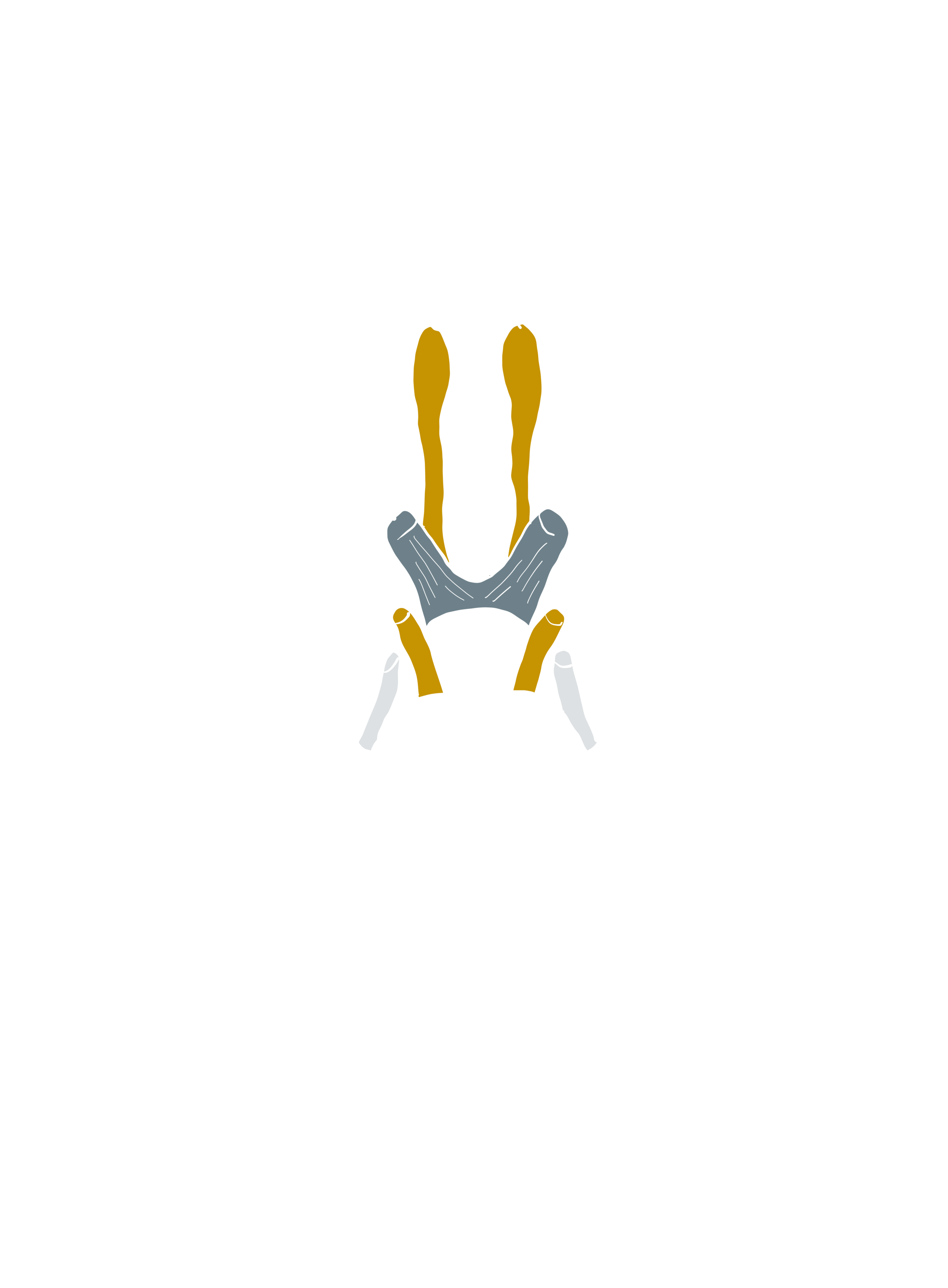
I Olfactory Nerve
The olfactory nerve transmits information to the brain regarding a person’s sense of smell.
When a person inhales fragrant molecules, olfactory receptors within the nasal passage send the impulses to the cranial cavity, which then travel to the olfactory bulb.
Specialized olfactory neurons and nerve fibers meet with other nerves, which pass into the olfactory tract.
The olfactory tract then travels to the frontal lobe and other areas of the brain that are involved with memory and notation of different smells.
II Optic Nerve
The optic nerve transmits information to the brain regarding a person’s vision.
When light enters the eye, it hits the retina, which contains rods and cones. These are photoreceptors that translate signals from light into visual information for the brain.
Cones are located in the central retina and are involved with color vision. Rods are located in the peripheral retina and are involved with non-color vision.
These photoreceptors carry signal impulses along nerve cells to form the optic nerve. Most of the fibers of the optic nerve cross into a structure called the optic chiasm. Then, the optic tract projects to the primary visual cortex in the occipital lobe at the back of the brain. The occipital lobe is where the brain handles visual information.
III Oculomotor Nerve
The oculomotor nerve helps control muscle movements of the eyes.
The oculomotor nerve provides movement to most of the muscles that move the eyeball and upper eyelid, known as extraocular muscles.
The oculomotor nerve also helps with involuntary functions of the eye:
The sphincter pupillae muscle automatically constricts the pupil to allow less light into the eye when the light is bright. When it is dark, the muscle relaxes to allow more light to enter.
The ciliary muscles help the lens adjust to short range and long range vision. This happens automatically when a person looks at near or far objects.
IV Trochlear Nerve
The trochlear nerve is also involved in eye movement.
The trochlear nerve, like the oculomotor nerve, originates in the midbrain. It powers the contralateral superior oblique muscle that allows the eye to point downward and inward.
V Trigeminal Nerve
The trigeminal nerve is the largest cranial nerve and has both motor and sensory functions.
Its motor functions help a person to chew and clench the teeth and gives sensation to muscles in the tympanic membrane of the ear.
Its sensory division has three parts that connect to sensory receptor sites on the face:
The ophthalmic part gives sensation to parts of the eyes, including the cornea, mucosa in the nose, and skin on the nose, the eyelid, and the forehead.
The maxillary part gives sensation to the middle third of the face, side of the nose, upper teeth, and lower eyelid.
The mandibular part gives sensation to the lower third of the face, the tongue, mucosa in the mouth, and lower teeth.
Trigeminal neuralgia is a common disorder of the trigeminal nerve that can cause intense pain and facial tics.
VI Abducens Nerve
The abducens nerve also helps control eye movements.
It helps the lateral rectus muscle, which is one of the extraocular muscles, to turn the gaze outward.
The abducens nerve starts in the pons of the brainstem, enters an area called Dorello’s canal, travels through the cavernous sinus, and ends at the lateral rectus muscle within the bony orbit.
VII Facial Nerve
The facial nerve also has both motor and sensory functions.
The facial nerve is made up of four nuclei that serve different functions:
movement of muscles that produce facial expression
movement of the lacrimal, submaxillary, and submandibular glands
the sensation of the external ear
the sensation of taste
The four nuclei originate in the pons and medulla and join together to travel to the geniculate ganglion.
Bell’s palsy is a common disorder of the facial nerve, which causes paralysis on one side of the face and possibly loss of taste sensation.
VIII Vestibulocochlear Nerve
The vestibulocochlear nerve is involved with a person’s hearing and balance.
The vestibulocochlear nerve contains two components:
The vestibular nerve helps the body sense changes in the position of the head with regard to gravity. The body uses this information to maintain balance.
The cochlear nerve helps with hearing. Specialized inner hair cells and the basilar membrane vibrate in response to sounds and determine the frequency and magnitude of the sound.
These fibers combine in the pons and exit the skull via the internal acoustic meatus in the temporal bone.
Cranial subluxations can result from trauma from falls, accidents or sports-related injuries. Other common causes include severe emotional stress, environmental toxins, a challenging birth or prenatal stress.
A Chiropractic evaluation which is performed during your first visit will consist of your Chiropractor assessing these cranial nerves as well as your body in order to help you on your Journey to health + wellness.
What To Expect At Your First Chiropractic Visit
An initial Chiropractic exam for back pain will typically have three parts: a consultation, case history, and physical examination. Laboratory analysis and X-ray examination may be performed.
Consultation. The patient meets with the chiropractor and provides a brief synopsis of his or her lower back pain, such as:
Duration and frequency of symptoms
Description of the symptoms (e.g. burning, throbbing)
Areas of pain
What makes the pain feel better (e.g. sitting, stretching)
What makes the pain feel worse (e.g. standing, lifting).
Case history. The chiropractor identifies the area(s) of complaint and the nature of the back pain by asking questions and learning more about different areas of the patient's history, including:
Family history
Dietary habits
Past history of other treatments (chiropractic, osteopathic, medical and other)
Occupational history
Psychosocial history
Other areas to probe, often based on responses to above questions
Physical examination. A chiropractor may utilize a variety of methods to determine the spinal segments that require chiropractic treatments, including but not limited to static and motion palpation techniques determining spinal segments that are hypo mobile (restricted in their movement) or fixated. Depending on the results of the above examination, a chiropractor may use additional diagnostic tests, such as:
X-ray to locate subluxations (the altered position of the vertebra)
A device that detects the temperature of the skin in the paraspinal region to identify spinal areas with a significant temperature variance that requires manipulation.
Chiropractors are trained in a variety of methods to assess the underlying cause of the problem, including:
Evaluation and management services. Chiropractors are trained in examining the joints, bones, muscles and tendons of the spine, head, extremities and other areas of the body with the purpose of noting any misalignment, tenderness, asymmetry, defects or other problems.
Neurologic and other common physical examination procedures. Chiropractors are trained to perform a variety of neurologic tests (nerve root compression/tension, motor strength, coordination, deep tendon and pathological reflexes, etc.) and are skilled in performing orthopedic, cardiovascular and many other common examinations.
Specialised assessment. Chiropractors are trained to assess range of motion, stability, muscle strength, muscle tone and other assessments with the lower back.
Common diagnostic studies. Chiropractors are trained in use of diagnostic studies and tools such as radiography (X-rays), laboratory diagnostics and neurodiagnostics.
References
1. https://www.medicalnewstoday.com/articles/326621#facial
2. https://www.ncbi.nlm.nih.gov/books/NBK470353/
3. https://teleemg.com/manual/cranial-nerves/
4. https://www.kenhub.com/en/library/anatomy/the-12-cranial-nerves
5. https://www.sciencedirect.com/topics/medicine-and-dentistry/cranial-nerve
6. https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-020-01134-1
7. https://anatomypubs.onlinelibrary.wiley.com/doi/full/10.1002/ar.23928
8. https://www.statpearls.com/ArticleLibrary/viewarticle/38677
9. https://www.physio-pedia.com/Cranial_Nerves
10. https://health.ucsd.edu/specialties/neuro/specialty-programs/pages/cranial-nerve-disorders.aspx
11. https://now.aapmr.org/cranial-nerve-visual-and-hearing-dysfunction-in-disorders-of-the-cns/
12. https://oxfordmedicine.com/view/10.1093/med/9780190259631.001.0001/med-9780190259631-chapter-21
13. https://www.frontiersin.org/articles/10.3389/fcell.2020.00635/full